HUAREN MEDICAL TECHNOLOGY
STEM CELLS
Stem cells in chronic wound healing
Trauma, burns, and many chronic diseases, such as diabetes and peripheral vascular disease, can lead to chronic refractory wounds. As the prevalence of obesity and diabetes rises, so does the incidence of chronic wounds. Such wounds pose a great challenge for clinical management and have a serious impact on the patient's image and psychology. Currently, treatments for chronic wounds include debridement, topical antibiotics, compression bandages, skin grafts, and growth factors. However, the therapeutic effects are not satisfactory, so there is an urgent need to explore new approaches.
Mesenchymal stem cells (MSCs) are a heterogeneous group of adult stem cells generated from embryonic connective tissue with self-renewal and multidirectional differentiation ability. Numerous studies have shown that stem cells can differentiate into cells at the site of damaged tissues and migrate to distant sites of injury to promote tissue repair. The roles of stem cells in chronic wound healing include cell recruitment, cell differentiation, immunomodulation, antimicrobial, pro-angiogenic, and epidermal replantation.
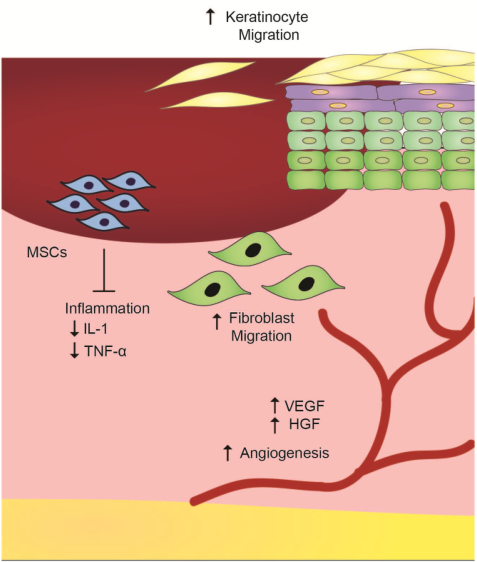
Figure 1 Mechanisms of stem cell action in wound healing
Pressure sores are ischemic injuries to soft tissues caused by unreleased pressure on a bony prominence and are prone to occur in patients who are bedridden for long periods of time. Stage III and IV pressure ulcers are less effective because they develop deeper ulcers. Some researchers have attempted to use stem cells to promote healing in advanced pressure sores. Twenty-two spinal cord injury patients from the Hospital Universitario Central de Asturias (Spain) suffered from stage IV pressure sores that lasted longer than four months.J González Sarasúa and team debrided the patients' deep wounds, followed by suturing the wounds to form a hollow bag, and then finally infusing bone marrow mononuclear cells extracted from the patients' bone marrow back into the bag.The number of cells infused in each infusion was 264.57×106±70.71 and were followed up at 1, 3, 6 months and 1 year after infusion. The results showed complete healing of the pressure ulcers in 19 out of 22 patients, 17 of whom received only a single stem cell infusion and showed wound closure after 3 weeks, as well as no recurrence during the follow-up period.
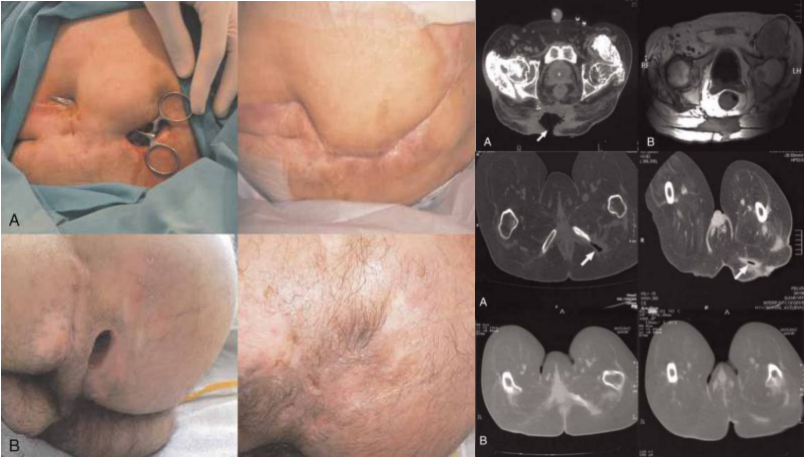
Figure 2 Gross observations and imaging comparisons of the two patients before and after transdermal stem cell infusion
Diabetic foot ulcer (DFU) is one of the complications caused by diabetes mellitus, which has a long healing time or even requires amputation. There have been numerous studies on stem cells to promote wound repair in DFUs.Zeng et al. extracted mesenchymal stem cells (PDMSCs) from placental tissue and mixed the stem cells with sodium alginate powder to form a gel-like PDMSCs complex. They then filled the complexes onto the entire wound surface (cell count: 1 × 106/cm2) of a 57-year-old patient with diabetic foot ulcers (The First Affiliated Hospital of Nanchang University) and covered it with a dressing, which was changed once a day for 3 weeks. Cefoperazone, sulbactam and insulin were also given for anti-inflammatory and glycemic control. The patients were followed up for 6 months. The results showed that foot pain decreased after 48 hours, local swelling decreased after 72 hours, granulation tissue appeared in the wound, and the wound healed completely after 3 weeks.
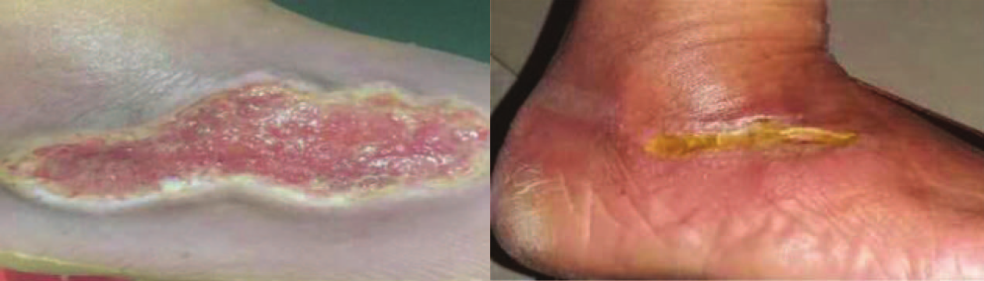
Picture 3 Before and after stem cell dressings to fill foot ulcers
Aurore Lafosse et al. extracted adipose-derived stromal cells (ASC) from the periumbilical adipose tissue of a patient (radionecrotic wound) and inoculated the cells onto lyophilised decellularised allogeneic broad fascia to form a biological dressing. After thorough debridement, the biological dressing was placed over the wound and secured with sutures to keep the cell layer in close contact with the wound, while the dressing was covered with petroleum jelly-impregnated dressing and changed daily. After 28 days of implantation, the biologic dressing is gradually absorbed leaving granulation tissue and the wound begins to heal.
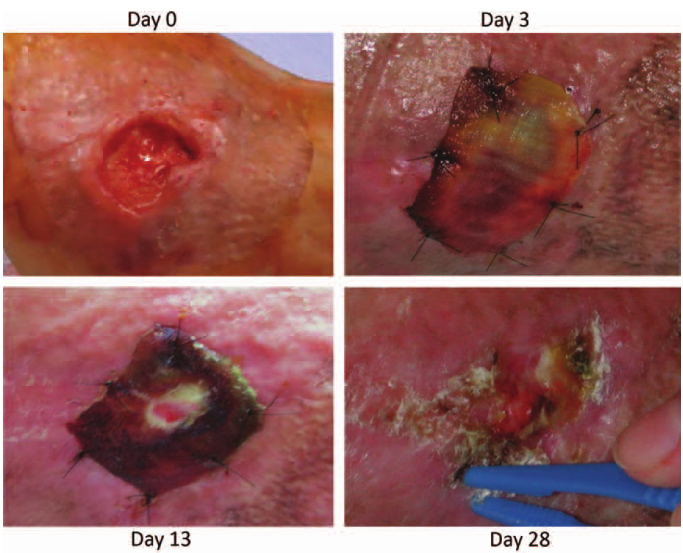
Figure 4 Evolution of a radionecrotic wound filled with a stem cell dressing
Stem cells have shown the potential to promote chronic wound healing and play an important role in the healing of chronic wounds such as diabetic ulcers, pressure sores, and radiation injuries. However, the role of stem cells in cancerous wounds has been less studied, probably because there is no direct evidence to prove whether stem cells have a promoting effect on tumour cells. In addition, most of the current studies have focused on basic research with fewer clinical reports, and the source of cells, dosage administered, time of administration, and route of administration need to be optimised by expanding the clinical sample size.